85 YEAR OLD MALE
DIVYA(2019 BATCH)
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
84 year old male came to the OPD with cheif complaints:
Sob since 3 days
Tightness of the chest since 3 days.
TREATMENT -
1)INTERMITTENT CPAP
2)HEAD END ELEVATION
3)FLUID RESTRICTION <2.5lts /day
4)SALT RESTRICTION <3 GMS /DAY
5)INJ LASIX 100MG IN 40 ML NS @5ml/hr
6)INJ DOBUTAMINE 1Amp
7)TAB CARVEDILOL 3.5 mg po/od
8)TAB ECOSPORIN GOLD 75/75/20 PO/0D
9)NEB WITH IPRAVENT 6TH HOURLY ,BUDECORT 8TH HOURLY
10)VITALS MONITORING
HOPI:
Patient was apparently asymptomatic 3 days back then he developed sob since 3 days MMRC grade 3 and wheeze which was aggravated on sitting and relieved by rest.
Orthoapnea present and no pnd
He also had tightness of the chest since 3 days with no aggravating and relieving factors
No c/o fever,cough, palpitations,hemoptysis .
Past illness:
K/c/o Hypertension since 20 years and on medication.
K/c/o CVA which occurred 20 years ago with left sided paralysis ( conservatively managed)
N/k/o DM,Epilepsy,Asthma,CAD,CKD,Tb.
H/o respiratory complaints of sob 2 months ago which was treated conservatively.
Treatment History:
On medication for Hypertension
TAB.LOSARTAN since 20 years.
Personal History:
Married
Occupation: farmer
Diet: mixed
Appetite: normal
Sleep: adequate
Bowel and bladder movements: regular
Addictions: alcoholic but stopped since 20 years.
Smokes 10 beedi's per day since 50 years
Allergies :no.
Family History: Nil significant.
General examination:
Moderately built and nourished
Height:
Weight:
BMI:
No pallor
No cyanosis
No icterus
No clubbing
B/L pedal odema Present
No lymphadenopathy
Temp:97°
Pulse rate:107
Blood pressure:
Respiratory rate:23
Systemic examination:
CVS:
S1S2 heard,no murmurs
RS:
Trachea: central
Dyspnea: present
Wheeze: present
Vesicular breath sounds heard
B/L rhonchi present.
Abdomen:
Shape: scaphoid
Non tender
No palpable masses felt.
Liver:non tender,not palpable
Spleen:non tender,not palpable
No bruits
No free fluid found
Bowel sounds: heard
CNS:
Concious
Speech: normal
No signs of meningeal irritation.
All sensations are intact
Motor system: normal
Local examination (respiratory system)
Inspection:
Upper respiratory tract
Nose:no nasal polyps,no dns
Oral cavity: tobacco stained.
Posterior pharyngeal wall: normal,not inflammed.
Lower respiratory tract
Shape of the chest: symmetrical and elliptical.
Position of teachea : central
Hoarseness: absent
Apex beat: not visible
No crowding of ribs,no drooping of shoulders and wasting of the muscles.
No usage of accessory muscles .
Spiniscapular distance equal on both sides.
Chest movements equal on both sides
No scars,sinuses, engorged veins,kyphosis,scoliosis.
Palpation:
All inspectory findings are confirmed.
Trachea central in position.
Apex beat felt at left 5 th. intercostal space.
Percussion :
Direct: resonant
Indirect: resonant
Ascultation:
BAE+,NVBS
B/K Diffuse coarse crepts.
B/L Rhonchi present in MA,AA,IAA
Investigations
Serology:
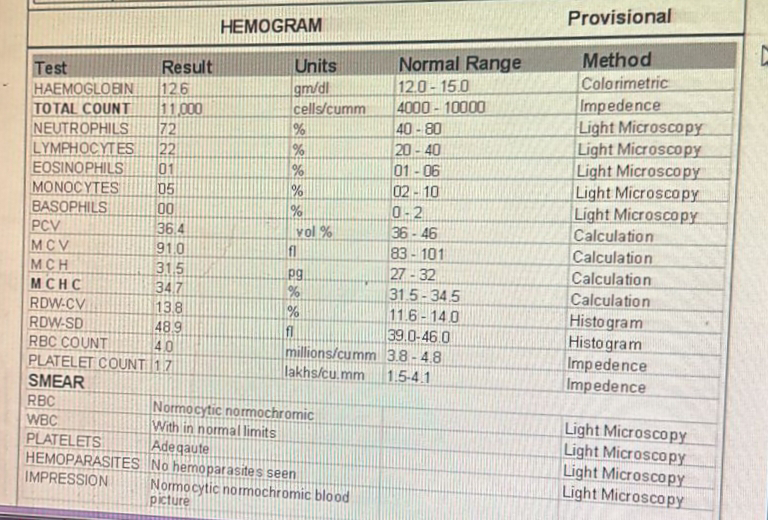
Hemogram
Arterial blood gas analysis
Renal function test
Hs-Troponin
ABG
ECG
1)Heart failure with reduced ejection fraction secondary to CAD(EF-25%)
2)CAD ACS STEMI With Cardiogenic Pulmonary odema.
3) Chronic kidney disease grade IV
4)Acute Exacerbation of Copd
5) H/o CVA RIGHT HEMIPARESIS(20YEARS BACK)
6)K/c/o HTN SINCE 20 YEARS.
7)Thrombocytopenia secondary to sepsis
TREATMENT:
1) Intermittent CPAP
2)HEAD END ELEVATION
3) Fluid restriction less than 2.5 litres per day
4) Salt restriction less than 2 gram per day
5)INJ.AUGUMENTIN 1.2 GRAM IV TID
6) INJ.DOBUTAMINE 1 AMPOULE IN 45ML NS( increase or decrease to maintain MAP</= 65 mmHg
7)INJ.LASIX 100MG IN 40 ML NS IV
8) TAB.AZITHROMYCIN 500MG PO/OD
9)TAB.ECOSPRIN GOLD 75/75/20 PO/OD
10)TAB.MET XL 12.5 MG PO/OD
11)SYP.CRIMAFFIN 10ML PO TID
12) NEBULIZATION WITH IPRAVENT @6HOURLY AND BUDECORT @12 HOURLY
13)BP,PR, TEMPERATURE @2HOURLY
14)STRICT I/O CHARTING
15)GRBS@7TH HOURLY PROFILE
16)INFORM SOS
17) INJ.HEPARIN 500 IU SC TID














Comments
Post a Comment